ENDOMETRIOSIS DIET
Women with endometriosis are frequently misdiagnosed with irritable bowel syndrome (IBS), crohn’s or ulcerative for some time before a correct diagnosis is made. Visceral hypersensitivity is a key feature in both conditions.
A connection between dietary factors and endometriosis onset has become a topic of interest mostly due to the observation that physiological and pathological processes of the disease can be influenced by diet.
Endometriosis is a hormone-dependent, chronic inflammatory gynaecological condition that causes pelvic pain symptoms impacting on the physical, mental and social wellbeing of reproductive-age women (Bianconi et al., 2007). Despite the high prevalence, which has been estimated to be between 6–10% (Parazzini et al., 1994) and the recognized economic burden associated with the disease (Simoens et al., 2012), its aetiology remains elusive. Various pathogenetic factors – menstrual, genetic, environmental, lifestyle – have been claimed to be implicated in the disease establishment and development (Viganò et al., 2004, Viganò et al.,2012).
The pathogenesis of endometriosis is repeated tissue injury and repair which leads to it’s hallmark features of neoangiogenesis and neoneurogensesis (new blood vessels and new nerve fibres ). The latter leads to hypersesnitization of the gastrointestinal nerves which manifest as an exaggerated response to a mild inflammatory stimulus. While a spicy bowel of curry might cause a little bit of indigestion in someone without endometriosis , it can render someone with endometriosis with severe pain and bloating because of the exaggerated response.
Endo belly is a term used to describe the uncomfortable, often painful, swelling and bloating that’s associated with endometriosis. Women complain of looking almost 20 weeks pregnant because of the painful abdominal distension, along with other symptoms like nausea, constipation or diarrhoea.
Hormonal pills or pain killers or antacids can reduce endometriosis symptoms and act as a temporary band-aid. Gut health is very important when it comes to endometriosis and is a synonym of mental and physical well-being including mood, sleep, cognition, pain etc., Although endometriosis is most likely an embryonically originated disease, it’s severity may progress with poor lifestyle and diet. Although data is limited there are many with endometriosis who found their symptoms to better with a properly “tailored” diet and some form of physical exercise.
Endometriosis is an estrogen dependent disease causing the levels of progesterone – the pregnancy hormone (required to make you fell calm, sleep better and successfully reproduce) to diminish. Hormones are these wonderful chemicals that keep every part of the body’s physiology in check. They regulate sleep, pain, hunger, reproduction, cognition, pH balance, blood sugar levels, heart rate, body temperature, growth of hair and nails, etc. and when their delicately balanced ecosystem is thrown out of balance, bad things happen!
There are different types of diets that are followed for endometriosis to better the symptoms. But a common thread among all of these are a few things to avoid such as:
- Refined sugars – that are in soda, canned drinks, toffees, cakes and sweets because sugar affects insulin- a hormone that has direct effects on estrogen levels and ovarian function (ovulation). Jaggery and honey are better alternatives
- Gluten – In a typical Indian diet we find gluten in wheat, maida and barley, the first two being the base or staple food in many parts of the world. Along with sugar, gluten tops the list of inflammatory foods. It also disturbs gut health and gut microbiota causing symptoms like bloating, constipation etc. that are seen with endometriosis. There are alternatives in the form of brown rice and quinoa.
- Trans fats Foods that usually contain high concentrations of trans fats include French fries, doughnuts, cookies/biscuits, chocolate, margarine, fried chicken and crackers. trans fatty acids are associated with higher circulating markers of systemic inflammation. Greater intake was associated with increased tumour necrosis factor system activity, with higher tumour necrosis factor receptor concentrations, higher concentrations of plasma IL-6 and C-reactive protein (Mozaffarian, 2006).
Good fats like ghee, avocados, nuts and eggs are good alternatives to highly processed foods.
- Red meat– we learn that intake of red meat, either as processed or unprocessed, is a major culprit in promoting endometriosis related symptoms . Replacement of red meat with fish, shellfish or eggs was associated with lower severity of symptoms. A quite unexpected result was the rise in endometriosis risk with increasing intake of poultry, albeit this was not as robust as seen for red meat. Yet another surprising finding is that the effect of red meat is independent of animal fat or its most common saturated fatty acid, palmitic acid and increase cholesterol levels. Substituting them with plant based proteins, fish loaded with anti- inflammatory omega 3 fatty acids and organic chicken can be helpful.
- Estrogenic foods – xenoestrogens and phytoestrogens are present in Soy.
Soy intake is common in Japan and in south-east Asia in general. In consideration of the link between endometriosis and oestrogens, it is conceivable that soy or, in general, phyto-oestrogen intake may be related with the risk of the disease. Broccoli, cauliflower, cabbage, red grapes, whole grains and flax seeds are good food options to regulate estrogen levels.
These are pretty much the foods to steer clear of.
Let’s take a look at the various diets available and analyse them
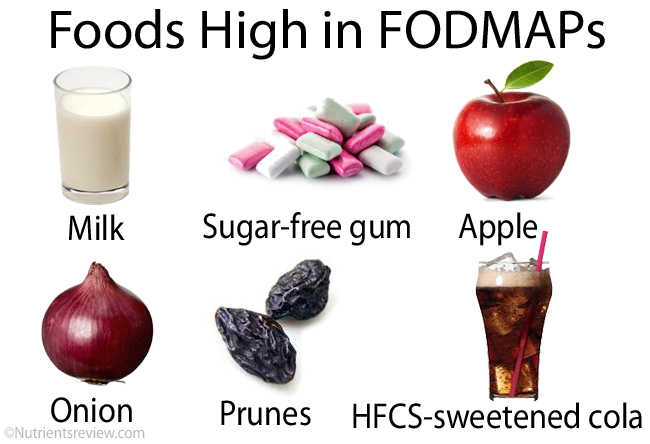
- The low FODMAPs diet: “fermentable oligo-, di-, mono-saccharides and polyols”
BACKGROUND: IBS / Irritable Bowel Syndrome manifests as bloating, abdominal distension and cramps, constipation and/ or diarrhea. Endometriosis is often misdiagnosed as IBS. Now connecting low FODMAPs with IBS brings us down to the science behind how FODMAPs disturb the gut. The first mechanism is high FODMAP foods are poorly absorbed by the small gut and they draw in water/ secrete water/fluid. This causes distension of the small gut which further leads to other abdominal symptoms and increased water delivery to the colon. The result is diarrhea. The second mechanism is high FODMAP foods are rapidly fermented by colonic microbiota leading to colonic distension. The manifestations are gas production, bloating and associated pain. This finally leads to constipation. It is a feedback loop and keeps circulating until that food which triggers isn’t removed.
FODMAPs expand to Fermentable oligo, di, mono saccharides and Polyols. They are present in the form of fructose in apples, pears, watermelons, lactose in dairy products, fructans in wheat, onion, garlic, galactans in legumes, soy milk and polyols in sorbitol, mannitol, xylitol, mushroom and pitted fruits.
Reducing or removing them all together could mean removing essential nutrients from your diet. So what’s the plan with the low FODMAP diet – with it not being a lifetime diet is to find out what foods triggers these symptoms by completely removing all high FODMAP foods from the diet and re introducing them one by one to find triggers. Identifying the triggers and and keeping them off the plate has proven to be beneficial in reducing and alleviating symptoms for people with both IBS and endometriosis. It takes around 6 weeks to actually identify the triggers. However, more research has to be done whether or not low FODMAP diet could prove useful for women with endometriosis alone.
- ELIMINATION DIET:
Elimination diet is similar to the FODMAP plan with a gradual reintroduction of trigger foods. Every person has different response mechanism for different types of trigger foods. So the mantra here, is to practice self awareness and mindful eating as to what foods trigger an inflammatory response. Since there can never be one size fits all diet, the elimination diet seems to be the best option .
- KETO DIET:
The keto diet works by severely restricting carbs and inducing a state of ketosis so that the body burns fat for energy. An ideal keto plate consists of 75% of calories coming from fatty foods like avocados, fish, eggs, ghee, nuts, spinach, lettuce, broccoli, cauliflower, mushroom, coconut oil, dairy etc., 20% of calories coming from protein from pulses, greens and less than 5% of calories coming from carbs in the form of onions, whole fruits. The reason why keto diet is so famous is that, it has proven scientifically to reduce body fat, LDL cholesterol, insulin resistance, estrogen levels and overall metabolism including sleep and excretion. Now, this is very important, the fact that there is reduction in the level of insulin and estrogen has made this diet really good for those with endometriosis. Regulated amounts of insulin and estrogen means a reduction of PMS like symptoms namely cravings, cramps, breast tenderness, mood swings, irritability etc. all of which contribute to better quality of life and wellness. But, whether or not this diet works for everyone without long- term side effects is still a question left unanswered.
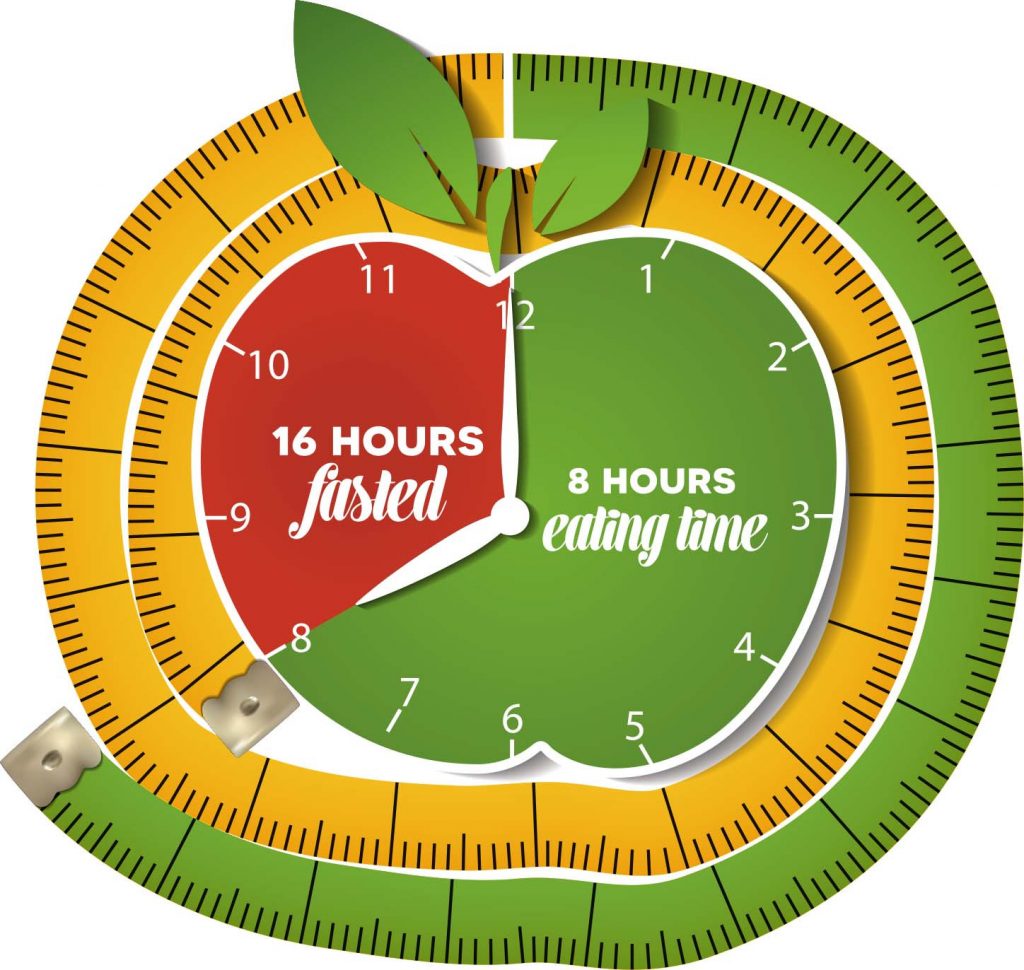
- INTERMITTENT FASTING DIET:
The IF diet is trending these days with those wanting to cut weight quickly. IF has several protocols like 14 hours to 16 hours a day or fasting for 2 days in a week or alternate day fasting. Claims of better quality of sleep after IF , increased energy throughout the day, better mood and cognition among others have been made, but the actual science of IF varies. People do generally fast when injured or sick, so that they can channel energy to repair cells or to fuel stem cells to heal and to make new cells. Since some people maybe sensitive to fasting or calorie deprivation, it is clinically advised to not stay more than 13 hours without eating anything.
Most diets targeted towards weight loss all work by creating a caloric deficit, but the problem is that some of them like keto or paleo or atkins tend to demonise certain food groups while others like intermittent fasting may not be very practical or sustainable long term.
In endometriosis, it is best to work with a nutritionist and self identification of foods that trigger inflammation. There is newer ongoing research into the gut “microbiome” and gut health which should yield promising insights in the days to come.
By Sagaya Kirti & Abhishek Mangeshikar