PAIN … More than just a four letter word
Pain is defined as an obnoxious sensory and emotional experience associated with tissue damage or inflammation or both. It may be acute pain (protective) or chronic pain ( all pervasive and destructive).
WHY DO WE HAVE PAIN?
It is an unpleasant but critical part of the body’s defensive system. It is a vital cog in the rapid warning and defence relay system by instructing the muscles via the brain to “move” to minimize the detected physical harm.
It is a sensory and emotional experience, generally associated tissue damage, or inflammation. Pain is ultimately a perception, and not an objective bodily state.
The unpleasantness of pain encourages organisms to use any means at its disposal to disengage from the noxious stimuli that it assumes cause the pain. It may, of course, have incorrectly determined the cause. Preliminary pain can serve to indicate that an injury is imminent, such as the ache from a “soon-to-be-broken” bone. Pain may also promote the healing process as most organisms will protect an injured region from further damage in order to avoid further pain. Despite its unpleasantness, pain remains an important part of human existence.
TYPES OF PAIN
- Acute
- Chronic
- Cutaneous (Skin)
- Somatic
- Visceral
- Phantom Limb
- Neuropathic
Pain is termed “nociceptive” when the clinical evaluation suggests that it is sustained primarily by the nociceptive system.
Nociceptive pain is pain that is proportionate to the degree of actual tissue damage. A more severe injury results in a pain that is perceived to be greater than that caused by a less severe injury.
Such pain serves a protective function. Sensing a noxious stimulus, a person behaves in certain ways to reduce the injury and promote healing (eg, pulling his finger away from a hot object). This “good” pain serves a positive function.
Some examples of nociceptive pain are acute burns, bone fracture, and other somatic and visceral pains.
Acute pain is defined as short-term pain or pain with an easily identifiable cause. Acute pain is the body’s warning of present damage to tissue or disease. It is often fast and sharp followed by aching pain. Acute pain is centralized in one area before becoming somewhat spread out. This type of pain responds well to medications.
Chronic pain is medically defined as pain that has lasted 6 months or longer. This constant or intermittent pain has often outlived its purpose, as it does not help the body to prevent injury. It is often more difficult to treat than acute pain. Expert care is generally necessary to treat any pain that has become chronic.
TYPES OF PAIN ACCORDING TO THE SOURCE
Cutaneous pain is caused by injury to the skin or superficial tissues. Cutaneous nociceptors terminate just below the skin, and due to the high concentration of nerve endings, produce a well-defined, localised pain of short duration. Example injuries that produce cutaneous pain include paper cuts, minor (first degree) burns and lacerations.
Somatic pain originates from ligaments, tendons, bones, blood vessels, and even nerves themselves, and are detected with somatic nociceptors. The scarcity of pain receptors in these areas produces a dull, poorly-localised pain of longer duration than cutaneous pain; examples include sprained ankle and broken bones.
Visceral pain originates from body organs visceral nociceptors are located within body organs and internal cavities. The even greater scarcity of nociceptors in these areas produces a pain usually more aching and of a longer duration than somatic pain. Visceral pain is extremely difficult to localise, and several injuries to visceral tissue exhibit “referred” pain, where the sensation is localised to an area completely unrelated to the site of injury. Myocardial ischaemia (the loss of blood flow to a part of the heart muscle tissue) is possibly the best known example of referred pain; the sensation can occur in the upper chest as a restricted feeling, or as an ache in the left shoulder, arm or even hand.
Phantom limb pain is the sensation of pain from a limb that one no longer has or no longer gets physical signals from – an experience almost universally reported by amputees and quadriplegics.
Neuropathic pain (“neuralgia”) can occur as a result of injury or disease to the nerve tissue itself. This can disrupt the ability of the sensory nerves to transmit correct information to the thalamus, and hence the brain interprets painful stimuli even though there is no obvious or documented physiologic cause for the pain.
Neuropathic pain occurs through central nervous system (CNS) changes, such as the processes of “wind-up” phenomenon and central sensitization that can occur in patients with a prolonged exposure to noxious stimuli or nerve injury, or through peripheral nervous system (PNS) changes, such as neuroma formation. It is disproportionate to the degree of tissue damage; it can occur without nociception.
Also called neurogenic pain, neuropathic pain occurs when pathophysiologic changes become independent of the inciting event, thus serving no protective function.
Neuropathic pain does not serve a positive function for the overall health of the person.
Some examples of neuropathic pain are painful diabetic and other peripheral neuropathies, deafferentation and sympathetically-maintained pains, and nerve inflammation, compression, or laceration.
Mixed pain In a given patient, components of continued nociceptive pain may coexist with a component of neuropathic pain. Patients with persistent back and leg pain following lumbar spine surgery (failed low-back-surgery syndrome) represent a common example. Some patients with complex regional pain syndrome (reflex sympathetic dystrophy or causalgia) may develop painful complications that are nociceptive (eg, joint ankylosis, myofascial pain) and that coexist with the underlying neuropathic pain.
Idiopathic pain may be defined as pain that persists without any identifiable organic lesions or as pain that is disproportionate to the degree of tissue damage.
NORMAL CENTRAL PAIN MECHANISMS
Nociception, is the physiological sense for perception of physiological pain. Nociception does not describe psychological pain.
Nociceptors are the free nerve endings of neurons that have their cell bodies outside the spinal column in the dorsal root ganglion and are named based upon their appearance at their sensory ends. These sensory endings look like the branches of small bushes.
The interpretation of pain occurs when the nociceptors are stimulated and subsequently transmit signals through sensory nuerons in the spinal cord, which releases glutamate, a major exicitory neurotransmitter that relays signals from one neuron to another and ultimately to the thalamus, in which pain perception occurs. From the thalumus, the signal travels to the cerebrum, at which point the individual becomes fully aware of the pain
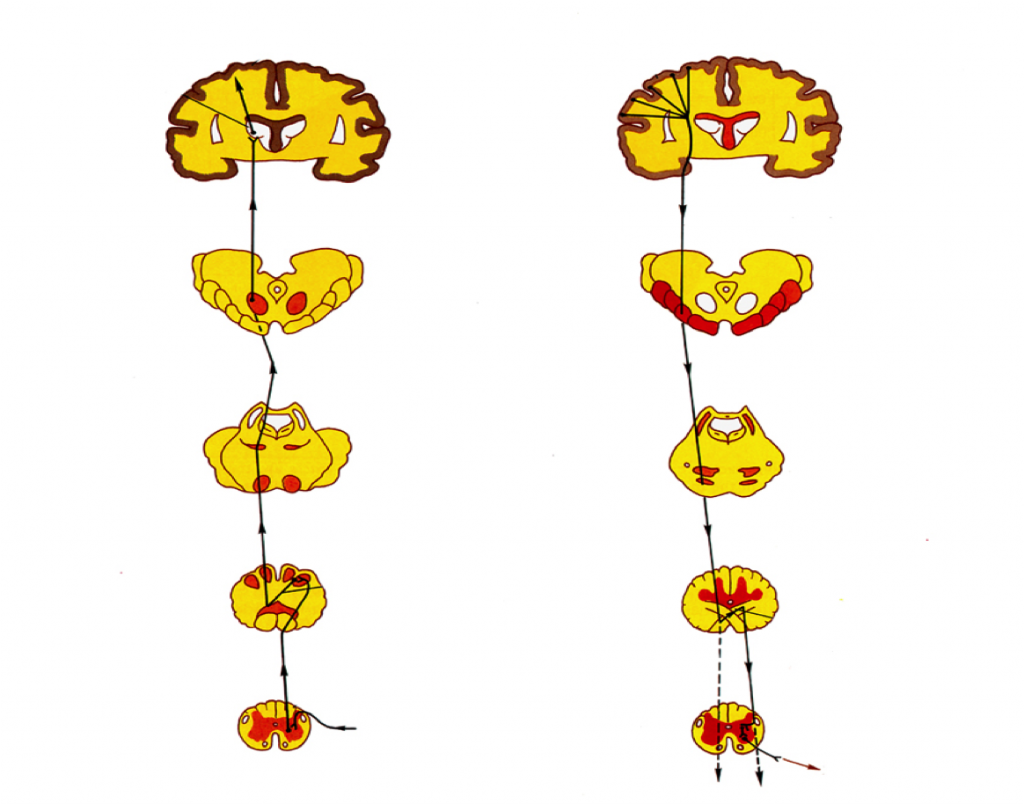
The nociceptive axon carries this impulse from the periphery into the dorsal horn of the spinal cord to make connections directly, and indirectly, through spinal interneurons, with second-order afferent neurons in the spinal cord.
The second-order neurons can transmit these impulses from the spinal cord to the brain. Second-order neurons ascend mostly via the spinothalamic tract up the spinal cord and terminate in higher neural structures, including the thalamus of the brain.
Third-order neurons originate from the thalamus and transmit their signals to the cerebral cortex.
Evidence exists that numerous supraspinal control areas—including the reticular formation, midbrain, thalamus, hypothalamus, the limbic system of the amygdala and the cingulate cortex, basal ganglia, and cerebral cortex—modulate pain. Neurons originating from these cerebral areas synapse with the neuronal cells of the descending spinal pathways, which terminate in the dorsal horn of the spinal cord.
MECHANISMS OF PATHOLOGICAL PAIN
A common peripheral source of pathophysiologic pain involves injured or diseased nerves.
Damaged nerves often grow axonal sprouts in which receptors to norepinephrine proliferate. These sprouts become highly sensitive to norepinephrine and thus to sympathetic nerve discharge. The nerves develop active sodium channels that become the sites of tonic impulse generation, known as ectopic foci.
These tonic impulses occur in primary nociceptive axons in the absence of a tonic nociceptive stimulus (eg, intense heat).
This abnormal tonic-impulse–input in nociceptors leads to central sensitization, an important concept in the pathophysiology of chronic pain.
Constant and/or intense bombardment of impulses from nociceptive afferents, particularly C nociceptive afferents, may lead to sensitization of dorsal horn neurons.
Sensitization of dorsal horn neurons leads to increased spontaneous impulse activity and their enhanced responses to impulses in nociceptive and even non-nociceptive primary afferents.
The consequences are hyperalgesia, allodynia, and spontaneous pain.
SINCE PAIN IS A MESSAGE TO THE BRAIN, THAT SOMETHING IS WRONG AND MUST NOT REMAIN, ONCE I HEAR ITS TALE OF WOE WHY THE HELL CAN’T IT JUST GET UP AND GO!
PAIN QUESTIONNAIRE
- Where is the pain?
- What does it feel like? throbbing, aching, burning?
- On a scale of zero to ten, with zero being no pain and ten being overwhelming pain, how bad is your pain now?
- When do you get this pain?
- What makes the pain better?
- What makes the pain worse?
- How is it affecting other parts of your life?
- Are you taking other medications for the pain, such as Aspirin, Paracetamol, Ibuprofen, Codeine, Morphine?
